The Role of HRA Data in Population Health
Healthcare providers have access to a wealth of insights, from clinical data to claims information, that can guide population health strategies. As vast as those data sets are, they can’t tell you everything about the communities you serve. According to the University of Wisconsin Population Health Institute, improving population health comes down to four factors:
- Healthcare, which accounts for 20% of population health improvements
- Physical environments, which account for 10%
- Behaviors, which account for 30%
- Social determinants, which account for 40%
Health risk assessments (HRAs) help you understand the full scope of risk factors impacting patient populations so you can create effective population health models. They provide you with insights into patient behaviors, physical environments, and social determinants, which account for 80% of the population health improvement factors listed above. By filling this critical data gap, you can create effective population health programs.
Source: Centers for Disease Control (CDC.gov)
How HRA Data Can Shape Population Health Programs
An HRA is a questionnaire that typically includes patient demographic information, emotional and physical health, lifestyle habits, and previous medical history. Successfully aggregating and analyzing HRA data enables you to target population health programs more effectively. For example, you can identify high-risk populations within dense urban areas and bring together local public and private resources to serve their specific needs.
Here are some of the most impactful ways to use HRA data.
1. Understand Social Determinants of Health
Social determinants of health (SDOH) refer to the conditions in the environments where people live, work, and play, and their impact on patient health. Examples of SDOH include home and workplace safety, transportation access, pollution, and access to healthy food. HRAs can be used to screen for SDOH, so providers can get a more comprehensive picture of their patient’s risk factors and barriers to care. For at-home care, HRAs commonly look for SDOH such as in-home safety hazards, transportation to specialized healthcare services, and access to healthy and nutritious foods.
2. Assess Change Readiness
Patient engagement is essential to creating effective population health programs. HRAs can include questions about how aware patients are of their risk factors and their willingness to change behaviors. Once you understand a patient population’s change readiness, you can create tailored programs that they’re more likely to engage with.
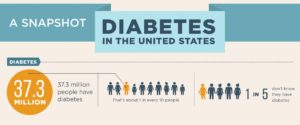
3. Watch for Signs of Chronic Diseases
Half of Americans suffer from chronic diseases, accounting for 86% of healthcare costs. HRAs allow you to watch for the early warning signs of chronic diseases like diabetes, kidney disease, and cancer. With that data, you can segment high-risk patients and recommend preventive strategies to reduce the progression of an illness.
Population Health Programs and Chronic Diseases
Chronic diseases are often avoidable. Population health programs can be the ideal vehicle for reducing the burden they place on the healthcare system. By closing the patient data gap with HRAs, you can implement effective strategies to improve patient outcomes. Some of the most promising ways to leverage this data to improve population health include:
- Educating the health workforce on the populations they serve, and their role in addressing population health
- Improving access to care by considering SDOH to ensure that services are patient-centered
- Expanding access to telehealth or at-home care services to streamline processes for providers and patients alike
These approaches target some of the most common roadblocks to preventing chronic disease and reducing the harm they cause. For example, diabetic patients can easily be overwhelmed by the sheer number of providers they need to see to manage the disease. However, since they’re managing their own illness most of the time, it’s important that they’re engaged in their own care. Population health providers can offer diabetic patient education, better access to care, and higher levels of convenience to help patients take more control of their health outcomes.
Connecting Patient Populations with the Right Care
One often preventable outcome of diabetes is diabetic retinopathy, which is the leading cause of blindness in adults. Through annual screenings, providers can identify diabetic retinopathy early and intervene to prevent the loss of sight. However, many patients don’t understand their risk factors or how often they should be screened.
In a recent study, half of the diabetic patients said they were unsure whether diabetes contributed to eye conditions such as cataracts, glaucoma, dry eye, and diabetic retinopathy. The study revealed that many patients felt there was a lack of coordination between their primary care providers and eye care providers. This points to a critical need for population health programs that not only close the education gap but also close the gaps between providers so patients can receive consistent, high-quality care.
Bridging the Gap with Technology
Technology is removing silos between providers and patients and making it easier to drive better outcomes. Innovative teleretinal imaging technology streamlines the retinal screening process so it’s easier for patients to receive preventive care for diabetic retinopathy. For example, handheld fundus cameras are allowing health risk assessment companies to screen for diabetic retinopathy in patients’ homes. Thanks to this device, a variety of providers, not just eye physicians, can perform retinal screenings in virtually any setting, allowing for the expansion of access to care.
At IRIS, we partner with population health managers and providers to make diabetic retinal exams more accessible. We work with you to understand the best ways to reach your patient populations and equip the healthcare workforce to end preventable blindness.
We’ve partnered with organizations like CommUnityCare in Texas to save the sight of thousands of patients. CommUnityCare works with an underserved population, and many of its patients live in rural areas. In addition to leading-edge retinal imaging cameras and board-certified eye specialists to review images, we provide them with a team that’s invested in their success. Read the case study to learn how IRIS’ client success team and training programs make it possible for CommUnityCare to reduce sight loss.
Partner with IRIS
Targeted chronic disease prevention programs offer an opportunity for population health managers to drive better outcomes in their communities. IRIS provides the technology and the support to help you make a real impact on saving patient sight. To learn about how other providers use IRIS, read our case studies.
If you’re ready to join us in the mission of ending preventable blindness, contact us for a consultation.
Population Health FAQs
What are the 4 components of population health?
The four components of population health are:
- Emphasis on primary care: Primary care physicians are the key to educating and empowering at-risk populations.
- Data-driven environment: Collecting and analyzing data is essential to understanding patient populations and measuring program effectiveness.
- Physician leadership: In order to reduce healthcare utilization, physicians need to be engaged in decision-making and planning.
- Off–the-radar disease management: It’s important to understand what patients do outside of the care facility (such as taking medication and exercising) to drive better outcomes.
What is meant by population health?
Population health refers to the health outcomes of a particular group of people. According to the CDC, it is a customizable, interdisciplinary approach geared towards addressing a patient population’s health challenges with effective policies and practices. The CDC released a Framework for Patient-Centered Health Risk Assessments (HRAs) where you can read more about how HRAs can help close patient care gaps.
Why is population health important?
Population health programs can improve outcomes for large groups of people, especially those who are typically underserved. Effective population health programs promote better patient engagement, reduce healthcare costs, and help to overcome some of the weaknesses in the healthcare system.
What are examples of population health?
Examples of population health programs include:
- Chronic disease management and prevention
- Pregnancy and maternal health
- Substance abuse prevention
- Vaccination awareness
- Reproductive health education
Why should healthcare providers implement HRAs?
HRAs help healthcare providers get a more comprehensive understanding of their patients. They close care gaps in existing patient datasets to help you understand behaviors, social factors, and readiness to change.
How does an HRA impact population health?
HRAs allow you to identify at-risk patients and target them with the right interventions. HRAs also open the gates to increased communication between patient and provider, leading to productive communication followed by action. By focusing your efforts on HRA data, you can improve outcomes while using resources wisely.
SM# 139, Rev A
Get started with IRIS today.
Want to know if IRIS is right for you? Schedule a one-on-one consultation with our team. We’re here to help.