What Factors Can Worsen Diabetic Retinopathy?

Diabetic retinopathy is one of the leading causes of preventable blindness in the U.S. and around the world. According to the Centers for Disease Control & Prevention (CDC), nearly 10 million Americans live with diabetic retinopathy, including 26% of all American diabetes patients. The CDC also reports that 1.8 million of those diabetic retinopathy patients have cases that are severe enough to threaten their vision, known as vision-threatening diabetic retinopathy (VTDR).
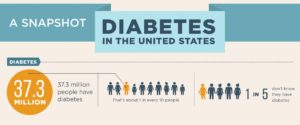
Source: Centers for Disease Control (CDC.gov)
There aren’t always noticeable symptoms during the early stages of diabetic retinopathy, so the disease often goes undetected until it’s too late. Without treatment, symptoms will gradually worsen over time. Various factors can speed up degeneration, such as elevated blood sugar levels and obesity. There’s even a link between common diabetes medications like Ozempic and diabetic retinopathy.
Preventative eye care, including regular eye exams and retinal screenings, is key to early detection of diabetic retinopathy. With early detection, treatments can be prescribed to slow or stop the progression. It can also help manage a patient’s diabetes care in a way that supports their eye health and ultimately spares their eyesight.
What Causes Diabetic Retinopathy?
Diabetic retinopathy is caused by elevated blood sugar levels that damage and degrade blood vessels in the retina. As a result, the blood vessels become swollen, leaky, or compressed so that blood is unable to pass through them to get to the retina, leading to the following:
- Blurry vision
- Dark spots, blank spots, and “floaters”
- Diminished night vision
- Macular edema
- Macular ischemia
In advanced cases, the retina may grow new blood vessels to compensate for the damaged ones, which can cause partial to full vision loss.
There are several diabetic retinopathy risk factors. A long history of diabetes is one, as well as unaddressed high blood sugar. Other risk factors include high blood pressure, high cholesterol, pregnancy, and smoking. Hispanic, Black, and Native Americans are also at greater risk of developing diabetic retinopathy.
What Are the Stages of Diabetic Retinopathy?
There are four stages of diabetic retinopathy:
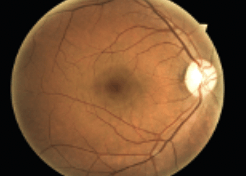
Normal Fundus
- Mild Non-Proliferative Diabetic Retinopathy (NPDR): The first signs of diabetic retinopathy are tiny microaneurysms in retinal blood vessels that cause them to swell. In most cases, this doesn’t affect vision.
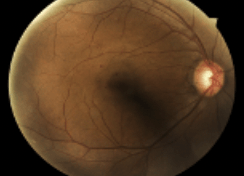
Mild NPDR
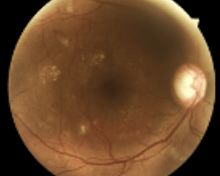
2. Moderate NPDR: As the disease progresses, blood vessels become damaged and leak blood and other fluid, impacting vision.
Moderate NPDR
3. Severe NPDR: During this stage, blood vessels become more damaged. This leads to increased swelling and leakage, further impacting vision.
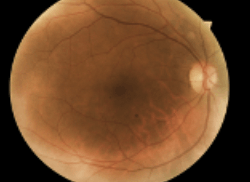
Severe NPDR
4. Proliferative Diabetic Retinopathy: In the final stages of diabetic retinopathy, the retina grows new blood vessels. This requires immediate treatment to stop the growth, shrink swollen blood vessels, and reduce leaking.
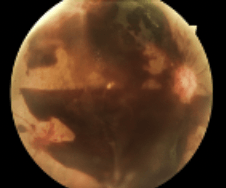
Proliferative Diabetic Retinopathy
What Causes Diabetic Retinopathy to Progress?
If left untreated, diabetic retinopathy can lead to complete vision loss. Treatments may include:
- Vascular endothelial growth factor inhibitors — injectable medicines that prevent the formation of new blood vessels
- Photocoagulation — laser treatments that shrink blood vessels and slow leaking
- Vitrectomy — the surgical removal of blood or scar tissue from the eye
Several factors can hasten the progression of diabetic retinopathy. Inadequate diabetes management, which fails to keep blood sugar levels within a healthy range, can increase the rate of progression. Obesity can also be a risk factor for diabetic retinopathy progression.
What is the Link Between Ozempic and Diabetic Retinopathy?
In recent years, a new risk factor has emerged: Ozempic, a medication commonly prescribed to help diabetes patients control their blood sugar levels. Ozempic, the brand name of the drug semaglutide, releases the GLP-1 hormone into the body, which jumpstarts insulin production. GLP-1 is the hormone that helps us feel full when eating, so Ozempic is also an effective weight management treatment.
However, studies indicate a negative correlation between Ozempic and diabetic retinopathy, suggesting potential complications of the condition. In some cases, diabetic retinopathy patients can experience undesirable Ozempic side effects that impair their vision and worsen their symptoms. This is due to the increased insulin production that Ozempic stimulates in the body. While the additional insulin is beneficial for regulating blood sugar levels, any changes in blood sugar can affect the eyes by altering the shape of the lens and impacting vision. Ozempic vision changes can include blurry vision and macular degeneration.

Other medications that produce the GLP-1 hormone can also accelerate the progression of diabetic retinopathy, but Ozempic poses a significantly greater risk. These medications include:
- Tanzeum
- Trulicity
- Victoza
- Metformin
The impact of Ozempic on diabetic retinopathy symptoms is generally short-term. Most patients experience Ozempic vision changes upon starting the medication, with symptoms typically lasting three to four months. Once vision returns to normal, patients often have an easier time managing diabetic retinopathy.
Improve Patient Care With Preventative Screenings
The IRIS solution helps healthcare providers safeguard their patients’ eyesight. With IRIS, doctors can provide cost-effective preventative retinal screenings to detect signs of diabetic retinopathy, facilitating early diagnosis so patients can immediately begin treatment.
IRIS can help you improve patient care. Reach out today to learn how.
FAQs
What Factors Can Worsen Diabetic Retinopathy?
Various factors can speed up the progression of diabetic retinopathy, such as elevated blood sugar levels and obesity. There’s even a link between common diabetes medications like Ozempic and diabetic retinopathy.
Can Ozempic Make Diabetic Retinopathy Worse?
Studies show that Ozempic can worsen diabetic retinopathy symptoms. Vision changes like blurry vision and enhanced macular swelling can occur. However, these side effects are not usually long-term.
How Does Ozempic Work?
Ozempic, or semaglutide, releases the GLP-1 hormone. Introducing GLP-1 into the body stimulates insulin production, which is crucial for stabilizing blood sugar levels.
Can Non-Diabetics Take Ozempic?
Yes, non-diabetics can take Ozempic. In fact, it’s sometimes prescribed to people with obesity instead of bariatric surgery because the GLP-1 hormone it releases gives the sensation of being full.
Does Ozempic Cause Eye Problems?
Yes, Ozempic can cause eye problems, according to studies. Ozempic stimulates insulin production, which changes blood sugar levels. Fluctuations in blood sugar levels can change the shape and size of the retinal lens. This can result in blurry vision. However, these eye problems generally last for only a few months.
SM 175, Rev A
Get started with IRIS today.
Want to know if IRIS is right for you? Schedule a one-on-one consultation with our team. We’re here to help.