How a Quick Eye Exam Can Detect Diabetic Retinopathy
It is estimated that 537 million people have diabetes globally. This means that the threat of diabetic retinopathy—the leading cause of vision loss in adults—is at an all-time high. However, some screening methods prevent the onset of blindness in adults with diabetes; from ophthalmologist screenings to a quick eye exam like teleretinal imaging. In this blog, we’ll further explore these diabetic retinopathy screening methods and see what tactics are being implemented to decrease the detection time of ocular conditions in eye exams.
Current Screening Methods
There are a few screening methods that have been developed for eye disease diagnosis. Each has its own processes, advantages, and disadvantages.
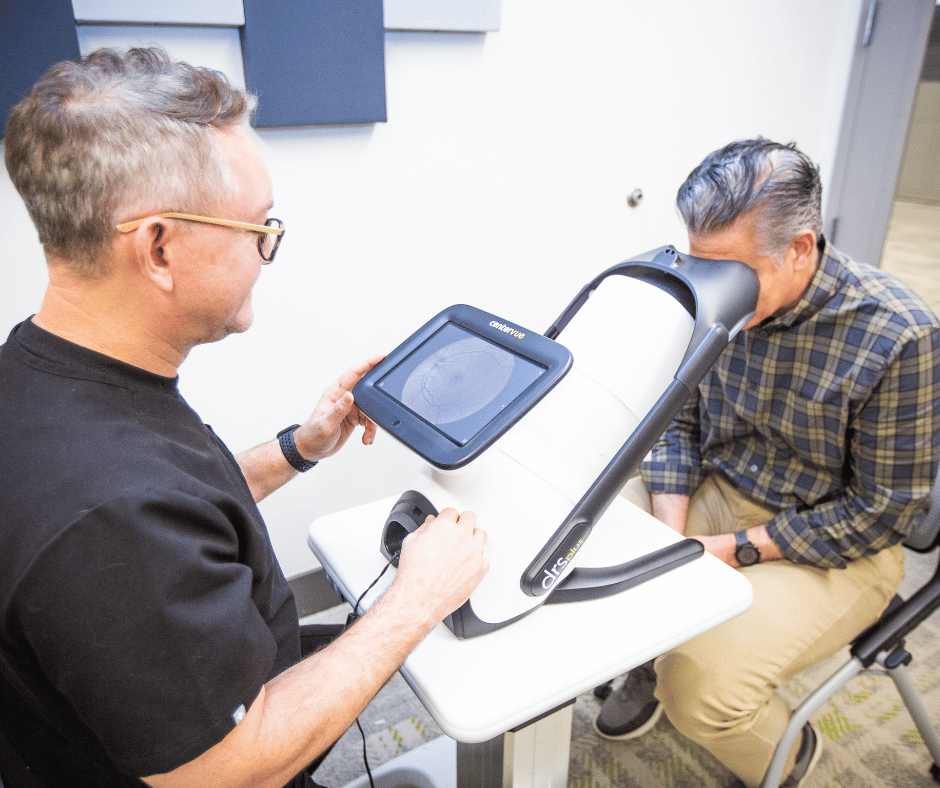
Teleretinal Imaging
Teleretinal imaging is the process of capturing and enhancing retinal images, then accurately diagnosing the presence of sight-threatening diseases like diabetic retinopathy. This solution is a cost-effective alternative to a fully dilated eye exam from an optometrist or ophthalmologist. Recent studies have found that fundus photography screenings like teleretinal imaging can save $127 per individual with diabetes when screened over their lifetime in populations with over 3,500 individuals aged 50 to 80. These cost savings were found with only 65% of individuals completing screenings.

Additionally, digital retinal imaging is a relatively quick eye exam, taking around five minutes and delivering results in two business days. The images are interpreted remotely by a licensed and trained physician to identify the presence of vision-threatening diseases and make an eye disease diagnosis.
Optometrist or Ophthalmologist Screening
Arguably the most common screening for diabetic retinopathy is an eye exam from an optometrist or ophthalmologist. In this screening, a physician will likely use eye drops to dilate a pupil and examine the back of the eye, otherwise known as the fundus. Sometimes the physician will take a photo of the back of the eye for further examination.
Screenings from optometrists or ophthalmologists take around 10 minutes and the results are delivered during the appointment. This type of screening is usually the result of a referral from a primary care physician. Unfortunately, this can lead to expanding care gaps. When patients have to schedule and attend multiple appointments, some of the traditional barriers to treatment including time and transportation exacerbate the problem and make it more difficult for at-risk patients to get treatment for diabetic retinopathy.
Fluorescein Angiography
Another test that is less common than the previous two is Fluorescein Angiography. In this test, a fluorescent dye is injected into a patient’s bloodstream. This illuminates the blood vessels in the fundus for easier examination. With diabetic retinopathy, blood vessels in the back of the eye are often damaged. If the fluorescence does not highlight blood vessels in the back of the eye, it can be a sign that a patient is suffering from a degenerative eye disease. This screening is not considered a quick eye exam. Although the examination only takes 15 to 20 minutes, the preparation and recovery from the test can last up to two hours.
Optical Coherence Tomography (OCT)
Optical Coherence Tomography (OCT) is a non-invasive eye exam that uses light to scan and take a cross-sectional retinal image. For diabetes-related eye conditions like diabetic retinopathy, OCT can detect damage to the small blood vessels of the eye without the need for injection of fluorescent dye, like with Fluorescein Angiography.
The downside of OCT is the cost of implementation. OCT equipment is not readily available outside of an ophthalmologist’s office. The upside is that OCT is a quick eye exam. In totality, the test takes between 5 to 10 minutes to complete, but the recovery from pupil dilation can take up to two hours.
Limitations of These Methods
Many of the limitations of making an accurate eye disease diagnosis with a quick eye exam come from the inability to close patient care gaps, especially those caused by social determinants of health. Because numerous screening methods require patients to go into a provider’s office for an examination, people afflicted by certain social determinants of health may have the physical inability to attend these screenings or may be unaware of their susceptibility to diabetic retinopathy.
As a solution to this, healthcare providers are turning to teleretinal imaging. This type of quick eye exam closes patient care gaps by providing tests inside and outside a primary care provider’s office, often directly in the patient’s home. With IRIS’s teleretinal screening solution, providers can begin closing care gaps for their patients by offering access to a retinal screening outside of the traditional eye care provider office.
How AI Can Make a Quick Eye Exam Even Quicker
While retinal photography is growing as a solution to closing patient care gaps, implementing Artificial Intelligence (AI) is promising to this sector in two distinct ways. First, AI is being used to grade fundus photography. By giving AI more power to grade fundus photography after a quick eye exam, physicians won’t have to take as much time to fully review teleretinal screenings. Instead, they could spend more time treating patients.

Second, AI is being used to detect patients at risk for diabetic retinopathy. With the help of Natural Language Processing (NLP), AI will be able to effectively identify patients susceptible to diabetic retinopathy by quickly sifting through large amounts of medical data. This will make it easier for healthcare providers to detect and treat diabetic retinopathy earlier, preventing vision loss from this condition with less invasive treatments and improving patient care overall.
Some of the current barriers associated with adopting AI for diabetic retinopathy on a widespread scale include implementation costs, patient confidentiality, and the need for more advanced and comprehensively trained technology. As of now, AI doesn’t provide a full diagnosis of diabetic retinopathy. Instead, it gives back refer, no refer, or ungradable results. This can lead to more time being spent making appointments with a specialist rather than just immediately seeing one or waiting two days for physician–interpreted results.
Opportunities for Diagnosing Diabetic Retinopathy With a Quick Eye Exam
As the need for better patient care continues to grow, healthcare providers will need to implement new processes that close patient care gaps and ensure equity across patient populations. The best way primary care providers can do this is by implementing the IRIS Solution into their patient care strategies.
With IRIS, retinal images are uploaded to the IRIS Reading Center (IRC), where remote physicians across the country look for signs of diabetic retinopathy within both the original and enhanced fundus images. The results from the IRC are sent directly to the patient’s EHR record, making it easier for providers to see the patient’s results as soon as they come in.
By implementing IRIS’s leading solution, healthcare providers can close patient care gaps with a quick eye exam and improve their HEDIS score. This helps gain more patients in the future, subsequently closing patient care gaps until vision loss in adults with diabetes is eradicated. To learn more about IRIS’s sight-saving mission, contact us, or schedule a demo to get in touch with a member of our team.
Frequently Asked Questions
How Does AI Technology Improve Diagnosis Rates?
AI technology improves diagnosis rates by processing and analyzing vast amounts of data at speeds beyond human capability. Machine learning algorithms are trained on thousands of medical records, enabling them to recognize patterns within dense amounts of patient data. This enhanced detection allows for early diagnosis of conditions like diabetic retinopathy and faster recognition of signs of diabetic retinopathy within fundus imagery.
Currently, AI does not have the capability of making complete diagnoses on a large scale. Today, there are only three results available with AI optionality: refer, no refer, and ungradable. These do not tell you what stage of diabetic retinopathy you may be in.
Can AI Help in the Screening of Eye Disease?
Yes, artificial intelligence (AI) can help in the screening of eye diseases. AI can be trained to recognize intricate details in fundus photographs, identifying early signs of conditions such as diabetic retinopathy or glaucoma. By offering limited results from screenings quicker, treatments can be implemented earlier, potentially preventing vision loss on a larger scale.
Is There Potential to Decrease Detection Time on Eye Exams?
Yes, there’s significant potential to decrease detection times during eye exams, thanks largely to fundus photography and teleretinal imaging. Compared to in-person appointments with optometrists or ophthalmologists, teleretinal imaging is a quick eye exam, only taking about five minutes. In addition, by sending fundus images to the IRIS Reading Center (IRC), retinal images can be reviewed for diagnosis of diabetic retinopathy by a remote physician with results often returning in less than one business day.
SM# 143, Rev A
Get started with IRIS today.
Want to know if IRIS is right for you? Schedule a one-on-one consultation with our team. We’re here to help.