How In-Home Healthcare Services Are Closing Patient Care Gaps

In today’s rapidly evolving healthcare landscape, ensuring that every patient receives timely, comprehensive, and effective care is paramount. Yet, despite the advances in the healthcare industry, significant patient care gaps persist. These gaps often create less equity for patients, especially ones who are high-risk, and prevent opportunities for early disease detection and diagnosis. This can lead to higher healthcare costs for both patients and providers, as well as poor health outcomes for people who need medical attention the most. One area of untapped potential, however, is in-home healthcare services.

In-home healthcare services aim to close patient gaps by providing personalized care that meets patients where they are, creating a system where healthcare accessibility and patient engagement are a priority. In this blog, we’ll explore how bringing healthcare directly to a patient’s home not only offers convenience but also bridges the lack of critical care many face. First, let’s start with refining our understanding of patient care gaps.
Understanding Patient Care Gaps
A patient care gap is any difference between what is a recommended best practice in healthcare and the treatment administered. For example, a patient care gap could be a recommended diabetic retinopathy screening for someone at risk due to their health conditions, such as diabetes. Unfortunately, these patients may not have access to care due to various social determinants of health that impact their lives.
In-home healthcare services are a way that medical providers can circumvent social determinants of health and meet patients where they are to close the gap in their access to care. Using diabetic retinopathy as an example again, providing an at-home screening for this disease can eliminate any barriers to treatment, including transportation, economic stability, community and environment, etc. In-home health services make convenience and accessibility a priority so patients don’t have to worry about any impediments to their treatment that may arise under traditional circumstances.

When healthcare providers decide to meet patients where they are with in-home healthcare services, it creates a cycle and culture for improving patient care that makes healthcare treatment more equitable for everyone.
The Virtuous Cycle of Improving Patient Care
Meeting Patients Where They Are
The first step in improving care with in-home healthcare services is meeting patients where they are. Every year, 3.6 million people in the U.S. are unable to receive medical care due to transportation issues. That number doesn’t even account for the 44% of Americans who can’t even afford to pay for healthcare. Eliminating barriers such as transportation and cost with in-home healthcare services makes getting treatment more accessible for everyone.

Closing Patient Care Gaps
When you meet people where they are, provide preventative screenings, and make healthcare treatment more accessible, you start to close patient care gaps. The treatment that these patients require is actually administered. This creates more opportunities to detect signs of underlying conditions early which can prevent hospital readmissions and more intense and expensive treatment in the future.
HEDIS & Star Ratings
After you start closing patient care gaps, your HEDIS and Star Ratings improve. The higher your score for both of these benchmarks, the better your patient care efficacy is. These numbers determine whether you’ve been properly treating patients and make it easier for you to receive funding, revenue, and reimbursement for your in-home healthcare services. Healthcare providers with low HEDIS scores and Star Ratings do not receive as much, or sometimes any, reimbursement.

Reinvestment for a Better Future
Once your HEDIS and Star Rating scores rise and you receive more funding, you can reinvest what you made to make your in-home healthcare services more affordable and efficient. When you continually optimize your in-home healthcare services, it creates a continuous feedback loop of better patient care. More funding means better treatment, which leads to better preventative care for patients and higher HEDIS and Star Ratings, which once again leads to more reimbursement.
What does that all mean? The cycle of closing patient care gaps not only benefits healthcare providers but also continuously benefits the patients that they’re treating over time.
Transforming In-Home Healthcare Services With the IRIS Solution
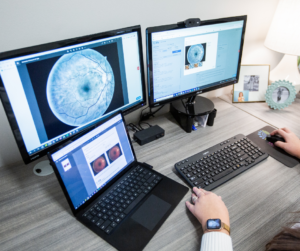
For in-home healthcare providers looking to take the next step in closing patient care gaps, the IRIS Solution may be the answer. IRIS’s preventative screening solution for diabetic retinopathy can integrate seamlessly with in-home healthcare providers’ EHRs, EMRs, and portable fundus camera technology, making it easier to administer sight-saving teleretinal eye exams.
When healthcare providers choose to integrate the IRIS Solution into their in-home healthcare services, it helps close care gaps, especially for those patients susceptible to the advancement of diabetic retinopathy. This closing of care gaps improves healthcare providers’ HEDIS and Star Rating, ensuring that they receive a reimbursement and reinvest their revenue into improving in-home healthcare services further.
To learn more about how IRIS is working to improve in-home healthcare services for all and how you can implement it into your healthcare system, schedule a demo or contact us. We’re working hard to close patient care gaps by ending preventable blindness, one screening at a time.
Frequently Asked Questions
How Can We Close the Gaps in Patient Care?
In-home health care offers a solution to close patient care gaps by providing continuous, personalized services directly to patients in their own environment. By addressing individual needs and reducing the barriers associated with in-office visits, home health care ensures more consistent and comprehensive care for patients.
What Is Gap Closure in Healthcare?
Gap closure in healthcare refers to the strategies and interventions aimed at bridging the disparities in patient care. It focuses on ensuring that every patient receives timely, appropriate, and comprehensive care, reducing the differences in health outcomes among different patient groups. By addressing these care gaps, healthcare providers enhance the overall quality and efficiency of medical services.
How Can a Healthcare Team Collaborate to Close the Gaps in the Provision of Quality Healthcare?
Healthcare teams can collaborate to close patient care gaps in in-home healthcare by utilizing telehealth platforms, sharing real-time patient information over EHRs, and working together to deliver continuous care and preventative screenings at home.
How Do You Address Gaps in Healthcare?
In-home healthcare addresses patient gaps by providing personalized care directly to patients in their own environment. This ensures continuity of care and reduces hospital readmissions. By bridging the space between hospital and home, in-home healthcare services can foster better patient outcomes and holistic well-being.
SM#155, Rev A
Get started with IRIS today.
Want to know if IRIS is right for you? Schedule a one-on-one consultation with our team. We’re here to help.